25 F with joint pains, facial puffiness, fever , weakness
This is an online E- log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box.
CONSENT AND DEIDENTIFICATION :
The patient and the attenders have been adequately informed about this documentation and privacy of the patient is being entirely conserved. No identifiers shall be revealed through out the piece of work whomsoever.
CHIEF COMPLAINTS
•25 YEAR OLD FEMALE, HOUSE WIFE BY OCCUPATION, RESIDENT OF NALGONDA CAME WITH THE CHIEF COMPLAINTS OF
•MULTIPLE JOINT PAINS SINCE 3 YEARS
•FACIAL PUFFINESS SINCE 2 WEEKS
•FEVER SINCE 5DAYS
•GENERALISED WEAKNESS SINCE 5DAYS
•AND HEADACHE SINCE 5DAYS
•SHORTNESS OF BREATH SINCE 3DAYS
HISTORY OF PRESENT ILLNESS
•PATIENT WAS APPARENTLY ASYMPTOMATIC 3 YEARS AGO THEN SHE DEVELOPED MULTIPLE JOINT PAINS INVOLVING LARGE AND SMALL JOINTS, WITH NO SWELLING OF JOINTS, INTERMITTENT IN NATURE,THEY USED TO DISTURB HER ROUTINE HOUSEHOLD ACTIVITES AND HAD NO MORNING STIFFNESS
•SHE DEVELOPED FEVER SINCE 15DAYS, HIGH GRADE FEVER ASSOCIATED WITH CHILLS AND RIGORS, INTERMITTENT IN NATURE, NO DIURNAL VARIATION RELIEVED ON TAKING MEDICATION
•NOT ASSOCIATED WITH COUGH
•ASSOCIATED WITH HEADACHE AND GENERALISED BODYPAINS – HEADACHE - FRONTAL REGION, INTERMITTANT IN NATURE , RELIEVED ON MEDICATIONS
•PATIENT WAS COMPLAINING OF SHORTNESS OF BREATH SINCE 3DAYS ON ORDINARY ACTIVITY, MAINLY DURING THE FEVER EPISODE, RELIEVED ON REST, NO DIURNAL VARIATION.
•NO ORTHOPNEA, PAROXYSMAL NOCTURNAL DYSPNEA, PROFUSE SWEATING, CHESTPAIN ,PALPITAIONS, WHEEZE.
PAST HISTORY
•K/C/O HYPOTHYROIDISM SINCE 5 YEARS ON TAB.LEVOTHYROXINE 25MCG/PO/OD
•H/O USAGE OF STERIODS FOR MULTIPLE JOINT PAINS SINCE 3YEARS
•H/O 3 ABORTIONS PREVIOUSLY – 2 IN FIRST TRIMESTER
• 1 IN 2ND TRIMESTER
•TWO COMPLETE SPONTANEOUS ABORTIONS IN FIRST TRIMESTER
•MEDICAL TERMINATION OF PREGANCY IN 2ND TRIMESTER AS FETAL HEART BEAT WAS ABSENT
•NOT A KNOWN CASE OF HYPERTENSION, DIABETES MELLITUS, CORONARY ARTERY DISEASE, CEREBRO VASCULAR ACCIDENTS, TUBERCULOSIS,ASTHMA OR SEIZURE DISORDER
•FAMILY HISTORY – NO SIGNIFICANT FAMILY HISTORY
PERSONAL HISTORY
•MIXED DIET
•SOUND SLEEP
•AQEDUATE APPETITE
•BOWEL AND BLADDER HABITS – REGULAR
•NO ADDICTIONS
GENERAL PHYSICAL EXAMINATION
•Patient is conscious, coherent and cooperative
Well oriented to time, place and person.
•Moderately built and Moderately nourished.
•Pallor and Anasarca present
•icterus, cyanosis, clubbing, lymphadenopathy
•JVP not raised
VITALS AT PRESENTATION:
•Blood Pressure: 130/70 mmHg, right arm in supine position
•Pulse Rate: 92 beats per min, regular, normal volume.
•Respiratory Rate : 20 cycles per min.
•Temperature: 100F
•SpO2 : 98% on Room Air
•GRBS: 132 mg/ dl
SYSTEMIC EXAMINATION
•RESPIRATORY SYSTEM:
INSPECTION
•Chest Is elliptical, bilaterally symmetrical
•Trachea is central in position
•Chest movements are symmetrical on both sides
•No scars.
•No visible pulsations
•Apical impulse not seen
PALPATION:
All inspectory findings are confirmed
No local rise of temperature
No Tenderness
Trachea is central ,chest movements are symmetrical on both sides
Tactile Vocal Fremitus: Normal in all areas
PERCUSSION:
•Resonant note heard in all areas.
AUSCULTATION:
•Bilateral air entry present
•Normal Vesicular Breath sounds heard
• No added sounds
SYSTEMIC EXAMINATION
CARDIOVASCULAR SYSTEM:
INSPECTION
•Elliptical and Bilaterally symmetrical chest
• Apical impulse not seen.
• Trachea appears to be central in position
•No visible pulsations/engorged veins/scars/sinuses on chest wall.
PALPATION
•Apex beat palpable at left 5th Intercostal space at midclavicular line.
•No palpable heaves, thrills present
•AUSCULTATION
•S1 and S2 normally heard.
•No murmurs heard.
SYSTEMIC EXAMINATION
•PER ABDOMEN :
•Scaphoid shaped
•No visible pulsations/engorged veins/scars/sinuses.
•Soft, Non tender.
•No guarding and rigidity.
•No organomegaly
•Bowel sounds present.
SYSTEMIC EXAMINATION
•CENTRAL NERVOUS SYSTEM:
Patient is Right handed
•Higher mental functions :Patient is oriented to time,place and person.
•Bilateral Pupils: Normal in Size and reacting to light.
•Cranial Nerves: Normal.
•Signs of Meningial
Sensory system - Normal
•Motor System : Power 5/5 in all 4 limbs.
• Tone – Normal in all 4 limbs
•Reflexes – Biceps Triceps Supinator Knee Ankle in both limbs
• ++ ++ + ++ +
•Plantors - Flexion in both limbs
JOINT EXAMINATION
•GENERAL APPEARANCE – NO SWELLING OR DEFORMITY
•INSPECTION – NO REDNESS,SCARS OR RASH
•ON PALPATION – NO EFFUSION , NO WARMTH ,TENDERNESS OR CREPITUS WERE PRESENT
•NO RESTRICTION OF MOVEMENT
PROVISIONAL DIAGNOSIS
MENINGITIS
•?ARTHROPATHY
• CUSHINGS SYNDROME
•ANEMIA
•HYPOTHYROIDISM
ECG
USG
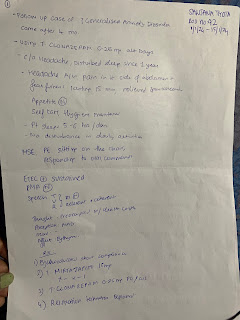
COURSE IN THE HOSPITAL
•25YEAR OLD FEMALE, HOUSEWIFE, RESIDENT OF NALGONDA PRESENTED WITH THE ABOVE MENTIONED COMPLAINTS TO THE CASUALTY
•H/O FEVER SINCE 5DAYS ASSOCIATED NECK STIFFNESS AND WAS SUSCPECTED TO HAVE MENINGITIS AND BLOOD AND URINE CULTURES WERE SENT
•ATTENDANTS DENIED FOR LUMBAR PUNCTURE
•IV ANTIBIOTICS WERE STARTED – INJ.MONOCEF 1GM IV BD
•AS CONTINIOUS FEVER SPIKES WERE PRESENT AND WITH RAISED TOTAL LEUCOCYTE COUNTS ANTIBIOTICS WERE ESCALATED TO
•INJ.PIPERACILLIN + TAZOBACTUM 4.5GM IV TID
•WITH USAGE OF STEROIDS FOR 3 YEARS
PATIENT WAS SUSPECTED TO HAVE STEROID
INDUCED CUSHING SYNDROME
TAB.PREDNISOLONE 5MG PO/OD
ANA PROFILE
ORTHOPEDIC OPINION WAS TAKEN FOR NECK PAIN AND ADVISED NO ACTIVE INTERVENTION FROM THEIR SIDE
•NEUROLOGIST OPINION WAS TAKEN AS PATIENT COMPLAINED OF NECK PAIN WITH STIFFNESS SINCE 3DAYS WITH B/L EYE ABDUCTION RESTRICTION AND WAS SUSPECTED TO HAVE RAISED INTRACRANIAL TENSION ?ASPETIC MENINGITIS ?BENIGN INTRACRANIAL HYPERTENSION
•MRI BRAIN, FUNDOSCOPY AND LUMBAR PUNCTURE WAS ADVICED
Xray Neck
MRI BRAIN
•AT THE TIME OF DISCHARGE FEVER SPIKES WERE ABSENT AND NECK PAIN WAS REDUCED, PATIENT WAS DISCHARGED IN HEMODYNAMICALLY STABLE CONDITION AND WAS ASKED TO REVIEW TO REVIEW TO GENERAL MEDICINE OPD AFTER 1 WEEK
DIAGNOSIS
•?SJOGRENS SYNDROME
•?SYSTEMIC LUPUS ERYTHEMATOSUS
•VASCULITIS WITH ACUTE INFARCT IN PONS
•CUSHINGS SYNDROME
•STEROID INDUCED NEPHROPATHY
•ANEMIA OF CHRONIC DISEASE (NORMOCYTIC-NORMOCHROMIC)
•HYPOTHYROIDISM
ADVICE AT DISCHARGE
•TAB. PREDNSIOLONE 5MG PO/OD ON FOR 5DAYS
•TAB.HYDROXYCHLOROQUINE 200MG PO/OD TO CONTINUE
•TAB. LEVOTHYROXINE 25MG PO/OD CONTINUE
•TAB.ECOSPRIN 75MG PO/OD TO CONTINUE
•TAB.DOLO 650MG/PO/SOS










Comments
Post a Comment