30 y/o female w/ SOB
This is an online E- log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box.
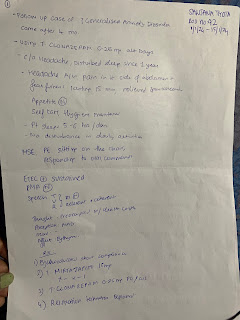
30 years old female presented to casualty with
chief complaints of sudden worsening of SOB since one day
History of presenting illness:
patient was apparently normal till six years back in 2017 she had generalised body aches and joint pains which involves multiple large joints of which elbow And knee joints troubled her associated with generalised body aches after multiple hospital visits
she even noticed hair loss without scarring and oral ulcers then she was diagnosed with autoimmune disorder and initiated on hydroxychloroquine azathioprine wysolone
she reported that her joint pains and hair loss was not improving with the above medication she had multiple hospital visits and admissions for joint pains and body aches which bothers her from doing her activities .
Two months back she had pedal edema two months back she had pedal edema sudden onset shortness of breath initially on exertion then she was diagnosed with hypertensive emergency admitted and discharged with antihypertensive . patients stopped AZA as advised by doctor except hyper antihypertensive since yesterday she had shortness of breath initially on exertion which rapidly progressed to sob at rest
No small joint pains no colour change /paraesthesia so fingers on exposure to cold
New onset of seizures :Patient had one episode of involuntary movements initially started left-hand followed by total body with impaired consciousness no tongue bite no involuntary maturation or defecation yesterday
Personal history:
daily routine a day starts at 7 AM after breakfast work starts from 9 AM attending client calls with 1 to 2 breaks in between till 6 PM more of sedentary work
Diet - mixed
Appatite-loss of appetite
Sleep- adequate
Bowel and bladder - regular
No Addictions
Past history :
Two months back she had pedal edema two months back she had pedal edema sudden onset shortness of breath initially on exertion then she was diagnosed with hypertensive emergency admitted and discharged with antihypertensive since 10 days .
Patient got dialysis done three times one month back
Insertion site : femoral region
O/e:
Patient conscious coherent cooperative
BP presentation to 220/140 MMHg given NTG and Nicardia ___BP-160/100 MMHg
PR-134bpm
RR-36cpm___24cpm
SpO2-236mg/dl
GRBS-236mg/dl
General physical examination :
Pallor present
flat nails
non-scarring alopecia
hyperpigmented discoid rashes on face Periauralblack discolouration of oral mucosa and palate
Mild pedal edema
CVS :
no raised JVP
S1 S2 +
no murmurs
RS:
BAE +
diffuse inspiratory and expiratory crepts
P/A:
Soft and non-tender
mild distended
umbilicus inverted
no organomegaly
CNS:
HMF intact
E4V5M6
Pupils NSRL
no FND(last seizure episode )
Labs :normocytic normochromic anaemia with leukocytosis
Diagnosis :
ACUTE CARDIOGENIC PULMONARY EDEMA with Immune mediated Glomerulonephritis.
SEIZURES SECONDARY TO ?PRES/?Uremia/? vasculitis.
Rx:
1.Inj. LEVIPIL 500mg IV TID
2.INJ.NTG 50 mg in 50 ml NS @5ml/hr to maintain SBP-<160mmhg
3. INJ.LASIX 40mg IV BD
4.TAB.NICARDIA RETARD 20mg PO BD
5.TAB.OROFER -XT PO/OD
6. Tab.HCQ 200mg PO BD
7.fluid and salt restriction
8. Monitor vitals and inform sos
9.INJ.HAI S/C acc to GRBS inform ICU /PG@ 7 point profile GRBS
10. Strict I/O Charting
11.TAB.MET XL 25mg PO BD
12. TAB.TELMA 40 mg PO/OD
13.TAB .WYSOLONE 20mg /PO/OD









Comments
Post a Comment