65 y/o male w/ anuria
This is an online E- log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box.
CONSENT AND DEIDENTIFICATION : The patient and the attenders have been adequately informed about this documentation and privacy of the patient is being entirely conserved. No identifiers shall be revealed through out the piece of work whomsoever.
CHIEF COMPLAINTS
A 65 y/o male presented to the casualty with chief complaints of fever since 4 days ago, not passing stool since 4 days. He had complaints of left sided abdominal pain since 2 days and vomiting (4 episodes) 2 days ago. He has not passed urine since 1 day.
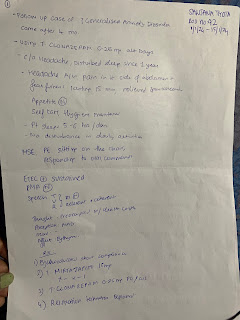
HISTORY OF PRESENTING ILLNESS:
The patient was asymptomatic 4 days ago and then he developed a low grade fever, relieved on medication, associated with chills, rigors and constipation. He had pain in the left hypochondriac region since 2 days ago, sudden onset, dull in nature and vomiting - 4 episodes - non projectile , non bilious. He had anuria since 1 day ago.
No history of burning micturition, cold, cough,
HISTORY OF PAST ILLNESS:
The patient is a known case of DM since 15 years- (glimiperide OD)
hypertension since 3 years (telmisartan, amlodipine,hydrochlorothiazide OD)
CUA since 2 years (stopped medication 2 months ago)
Bilateral tingling sensation in both lower limbs since 15 months.
PERSONAL HISTORY
Diet- Mixed
Appetite- Normal
Bowels and bladder- irregular, not passing stool and urine .
Sleep- adequate
Addictions- occasionally takes alcohol
FAMILY HISTORY
No significant family history
GENERAL EXAMINATION
Patient was conscious, coherent and cooperative, well oriented to time, place and person.
He is moderately built and nourished,
Vitals
BP-110/70
Pulse- 92 bpm
Respiratory rate-
Temperature- febrile
Pallor: absent
Icterus: absent
Cyanosis: absent
Clubbing: absent
Pedal edema: absent
Lymphadenopathy: absent
SYSTEMIC EXAMINATION
CVS: S1,S2 heard
RS: BAE +
CNS: Rt Lt
Tone: UL N N
LL N N
Power:
UL 5/5 2/5
LL 4/5 3/5
Reflexes:
Rt: Lt:
Biceps: ++ ++
Triceps: ++ ++
Supinator: ++ ++
Knee
Ankle
Plantar: flexor
GIT: on palpation, the abdomen was soft, tenderness in the left hypochondriac and left iliac region.
Investigations
CBP, CUE
2D echo
ECG
USG - chest
MRI brain
Provisional Diagnosis:
Prerenal AKI with viral pyrexia
Treatment:









Comments
Post a Comment