My Journey as an Intern In Medicine
“To cure sometimes, to relieve often, to comfort always.”- Edward Livingston Trudeau.
1) Self Reflection on my Medical Career:
My first case taken in the manner if an e-log during my 2nd year Medicine Posting.
https://sanjanathotarollno141.blogspot.com/2022/09/a-70-yr-old-female-with-involuntary.html?m=1
Through this process, I learned how to document the process of history taking, diagnosis, investigations and the treatment of a patient.
During my internship, I came across cases such as DKA, Heart Failure, CKD, SLE, Septic Shock,CVA, Epilepsy and common chronic diseases such as Diabetes, Hypothyroidism and Hypertension. I witnessed an episode of GTCS and the acute management of such a case in the ICU. I also learned how to diagnose and further evaluate a case of MI / ACS.I learned about spinal cord lesions, how to perform a full CNS examination and how to localize a stroke.
My journey in medicine as an intern was eye opening to say the least. I found myself learning from not only my seniors but also from patients’ and their relatives.
I learned the importance of communication, ethics and developing a good doctor- patient relationship. I learned the importance of maintaining confidentiality and building trust.
I found myself growing eager to learn how to come to a diagnosis from a list of differentials. I learned that there are many ways to take a full history and how important a proper history and physical examination is in terms of coming to a definitive diagnosis and allowing for more efficient management . I learned how important it is to take a full in depth history as many seemingly minor events can point to the main underlying cause of the patient’s current suffering
I learned the importance of understanding a patient’s lifestyle, their daily routine and their diet and how these factors shape the biopsychosocial factors that contribute to the patient’s disease course.
I learned how chronic illness affects those living in rural communities and how a long stay in the hospital affects their families financially and personally.
I also was made aware of the importance of good decision making skills and the need for good clinical skills to make the process of diagnosis and treating a case much simpler and more streamlined.
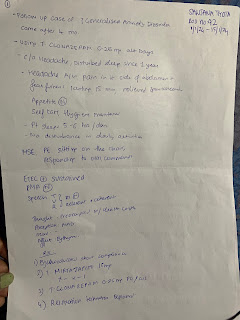
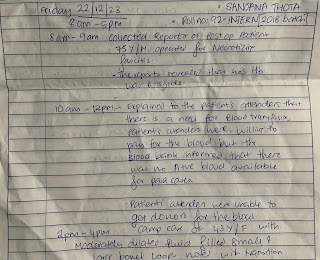
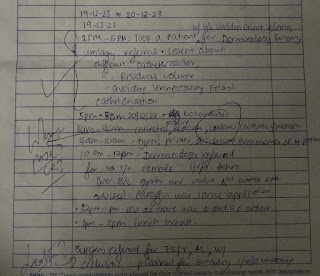
2) Evidence Based Daily Work logs.
1/12/23 - 15/11/23 Peripherals (ICU, Nephrology, Ward)
16/12/23- 31/12/23 Unit Duty
1/1/24- 15/1/24 - Psychiatry Posting
15/1/24- 31/1/24 - Unit Duty
My time as an Intern posted in the GM department started off in the Peripherals.
In the ICU:
- Monitored vitals
- Learned how to draw ABG samples
-Foleys Catheterization
-Ryles Tube Insertion
- Assisting Intubation of Critical Cases
- Monitoring Intubated patients
- Assisting during CPR
- Assisting during dressings
was exposed to critical cases and was faced with death on many occasions, I had the opportunity to learn how to manage critically ill patients, how to monitor patients who are hemodynamically unstable, how to communicate with both patients and their relatives.
Nephrology:
-Learned about Dialysis
-Central Line insertion- assisted
- Foleys Catheterisation
I learned about how chronic illnesses affect the daily lives of patients and how CKD disrupts the daily routines of both the patients and their families, spending days at a stretch at the hospital.
Ward:
- Learned about how the Medical ward ecosystem works, the rationale behind prescribing medication and investigations.
- Learned how to deal with any acute situations in the ward- Hypertensive emergencies, Febrile episodes.
- Ascitic tap
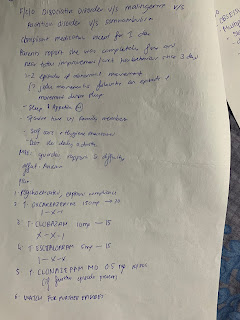
Psychiatry Posting:
- Learned how to take a detailed psychiatric history and make patients feel more comfortable. Learned about the importance of building a strong patient doctor relation, rapport , ethical issues regarding confidentiality.
- I learned about:
- Major Depressive Disorder
- Adjustment Disorder
- Schizophrenia
- Alcohol Dependence Syndrome
- Tobacco Dependence Syndrome
- OCD
- Somnambulism
-Marital issues counselling
Unit Duty
I learned the management of common cases seen in the OP- chronic illnesses such as DM, HTN, Hypothyroidism- including the relevant history and physical examination.
- Learned how to assess patients in the casualty and subsequent management.
- Learned how to counsel patients and communicate effectively to build a good doctor patient relationship
- learned about ethical prescription, appropriate investigations to avoid unnecessary financial burden to patients who are unable to afford them.
- Learned about the entire process from history taking , referrals, to the discharge process and staying in contact with patients so they are able to return for effective follow up.
Blogs:
Workflow
https://sanjanathotarollno141.blogspot.com/2024/01/65-f-with-aki-on-ckd-gastroenteritis.html?m=1
https://sanjanathotarollno141.blogspot.com/2024/01/35f-diabetic-with-vomitings-pain.html?m=1
https://sanjanathotarollno141.blogspot.com/2023/12/28-y-o-male-with-acute-diarrhea.html?m=1
https://sanjanathotarollno141.blogspot.com/2024/01/80-ym-with-fever-bl-lower-limb-weakness.html?m=1
https://sanjanathotarollno141.blogspot.com/2023/12/45-yo-male-with-acute-on-chronic.html?m=1
https://sanjanathotarollno141.blogspot.com/2023/12/54-yo-male-with-cld-subacute-intestinal.html?m=1
https://sanjanathotarollno141.blogspot.com/2023/12/60-yo-male-with-hypertension-heart.html?m=1
PAJR:
https://chat.whatsapp.com/Lb8fjkNMUlS6gf9CdRebpi
https://chat.whatsapp.com/LtsIC2jyN616QMFvG2ruKg
3)Anecdotal self reflections on their internship learning with some video evidence of procedures performed
Procedures Performed/ Assisted:
4) CASE BASED OSCE :
DKA : Mechanism Behind DKA:
Insulin deficiency, increased insulin counter-regulatory hormones (cortisol, glucagon, growth hormone, and catecholamines) and peripheral insulin resistance lead to hyperglycemia, dehydration, ketosis, and electrolyte imbalance which underlie the pathophysiology of DKA.
Hyperglycemia of DKA evolves through accelerated gluconeogenesis, glycogenolysis, and decreased glucose utilization – all due to absolute insulin deficiency. Of note, diabetes patients who developed DKA while treated with SGLT-2 inhibitors can present without hyperglycemia, i.e., with euglycemic DKA. Due to increased lipolysis and decreased lipogenesis, abundant free fatty acids are converted to ketone bodies: β-hydroxybutyrate (β-OHB), acetoacetate, and acetone. Hyperglycemia-induced osmotic diuresis, if not accompanied by sufficient oral fluid intake, leads to dehydration, hyperosmolarity, electrolyte loss, and subsequent decrease in glomerular filtration. With decline in renal function, glycosuria diminishes and hyperglycemia/hyperosmolality worsens. With impaired insulin action and hyperosmolality, utilization of potassium by skeletal muscle is markedly diminished leading to intracellular potassium depletion. Also, potassium is lost via osmotic diuresis causing profound total body potassium deficiency. Therefore, DKA patients can present with broad range of serum potassium concentrations. Nevertheless, a “normal” plasma potassium concentration may indicate that potassium stores in the body are severely diminished and the institution of insulin therapy and correction of hyperglycemia will lead to future hypokalemia.
Source: https://www.ncbi.nlm.nih.gov/books/NBK279146/#_diab-ketoacidosis_toc-pathophysiology_
Ketone Pathway:
Ketogenesis occurs primarily in the mitochondria of liver cells. Fatty acids are brought into the mitochondria via carnitine palmitoyltransferase (CPT-1) and then broken down into acetyl CoA via beta-oxidation. Two acetyl-CoA molecules are converted into acetoacetyl-CoA via the enzyme thiolase; this is also known as acetyl coenzyme A acetyltransferase (ACAT). Afterward, acetoacetyl-CoA is converted to HMG-CoA via the enzyme HMG-CoA synthase. HMG-CoA lyase then converts HMG-CoA to acetoacetate. Acetoacetate can be converted to either acetone through non-enzymatic decarboxylation or to beta-hydroxybutyrate via beta-hydroxybutyrate dehydrogenase.
Acetoacetate and beta-hydroxybutyrate are the two ketone bodies used by the body for energy. Once they reach extrahepatic tissues, beta-hydroxybutyrate is converted to acetoacetate via the enzyme beta-hydroxybutyrate dehydrogenase, and acetoacetate is converted back to acetyl-CoA via the enzyme beta-ketoacyl-CoA transferase. Acetyl-CoA goes through the citric acid cycle, and after oxidative phosphorylation, produces 22 ATP per molecule. Acetone does not convert back to acetyl-CoA, so it is either excreted through urine or exhaled.
https://www.ncbi.nlm.nih.gov/books/NBK493179/
OSA - Grades AHI
https://aasm.org/resources/factsheets/sleepapnea.pdf
Ankylosing Spondylitis- Sacro iliac joints
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4585948/
Tachyphylaxis Noradrenaline-
When to start Noradrenaline infusion-
For adults with septic shock on vasopressors, we recommend an initial target mean arterial pressure (MAP) of 65 mm Hg over higher MAP targets.
Extubation Criteria:
The most important part of this assessment is assessing the ability of the patient to protect and maintain a patent airway.
- The patient should have an adequate level of consciousness - a GCS greater than 8 suggests a higher likelihood of successful extubation.
- The patient should have a strong cough:
- Most clinicians objectively determine the presence of a moderate to strong cough before extubation, although there are other objective measures like card moistening and spirometry testing for maximal expiratory pressure (MEP).
- The presence of a weak cough, measured as a cough peak flow of 60 L/min or less, is a strong independent risk factor for extubation failure.
- The patient should be assessed for the volume and thickness of respiratory secretions.
- The most common test for airway patency is the cuff-leak test which is neither sensitive nor specific.
- Providers need to ensure that they know the airway anatomy noted at the time of intubation, potentially difficult airway, and techniques used to intubate the patient - in the case of the known difficult airway, ensure to have all equipment available for difficult airway. If extra personnel is needed, they should be informed beforehand and be available at very short notice.



















Comments
Post a Comment