28 Y /O MALE WITH ACUTE DIARRHEA
This is an online E- log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box.
CONSENT AND DEIDENTIFICATION : The patient and the attenders have been adequately informed about this documentation and privacy of the patient is being entirely conserved. No identifiers shall be revealed through out the piece of work whomsoever.
Patient came with c/o loose stools since 8 days, vomitings since 2 days, decreased appetite since 4 days.
Patient was apparently asymptomatic 8 days back and then developed loose stools, insidious in onset, gradually progressive, 2-3 episodes per hour, watery in consistency non foul smelling, non blood stained, no pus,
H/o 2 episodes of vomitings 5 days prior to admission, non projectile, non bilious, subsided.
HOPI
No h/o fever, cold, cough
No h/o chest pain, breathlessness, palpitations, syncope
No h/o pain abdomen, burning micturition
Past History
Not a k/c/o DM, HTN, asthma, thyroid disorder,seizure disorder, cad,cva.
Personal History
The patient is a resident of Chityala, plexi designer by occupation. Patient is exposed to unkown toxins during his daily work.
Appetite is lost, regularly eats food from outside , regularly consumes alcohol 90 ml / day.
loose stools since 8 days, 2-3 episodes per hour.
Non smoker
No h/o tobacco and drug use
Family History:
No significant family history
Physical Examination
General:
No Pallor, icterus, cyanosis, koilonychia, lymphadenopathy, edema.— Edema developed on 27/12
Temperature: Afebrile
PR: 89
RR: 15
BP: 80/60 mm Hg
GRBS: 115 mg /dl
P/A
Scaphoid , non tender, no palpable mass, free fluid, hernial orifices are normal, no bruits, no organomegaly.
CNS
Reflexes normal
No FND
CVS
S1 S2 Heard No murmurs
RS:
BAE +, NVBS heard
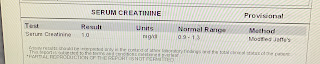
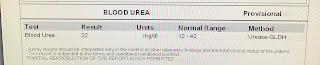
Investigations:
Stool Microscopy
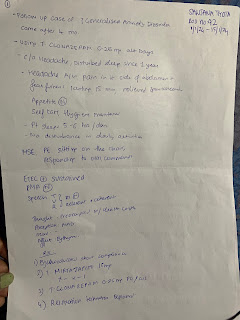
Treatment
IV FLUIDS RL , NS at 75 ml/hour
With 1 amp OPTINEURON
INJ CIPROFLOXACIN 200 mg IV BD
INJ METROGYL 500 mg IV TID
INJ PAN 40 MG IV OD
INJ ZOFER 4 mg IV SOS
ORS SACHETS
CAP REDOTIL 100 mg po bd
TAB SPORLAC DS PO TID
INJ NEOMOL 1 gm IV SOS
TAB DOLO 650 PO TID




Comments
Post a Comment