54 Y/O MALE WITH CLD, Subacute Intestinal Obstruction, Alcohol Dependence
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings investigations and come up with diagnosis and treatment plan.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings investigations and come up with diagnosis and treatment plan.
Chief Complaints:
Patient was brought to the casualty with c/o 2 episodes of vomitings since morning on 16/12/23
and c/o distension of the abdomen since 3 months.
c/o shortness of breath since 3 days
no h/o fever, decreased urine output, chest pain, palpitations
o/e:
Icterus +. Muscle wasting +
HOPI:
Patient was apparently asymptomatic about 3 months ago, then he developed pain abdomen, distended abdomen for which he was diagnosed and treated as with CLD, ascites and jaundice.
Now he c/o abdominal distension and protruded umbilicus associated with 2 episodes of non projectile, non bilious, liquid in content with no blood in in the vomitus. Patient has h/o usage of herbal medicine 2 months back. No h/o diarhoea or bleeding p/r, or burning micturition.
PAST HISTORY:
N/K/C/O DM, HTN, CAD, CVA, EPILEPSY
No history of previous surgeries, or blood transfusions.
Hospitalised 6 months ago i/v/o jaundice, ascites- referred to a higher centre
Swelling of the abdomen on and off since last 5 months, abstinent from alcohol since last 5 months.
Personal History:
Married
Occupation: Borewell digger/ tractor driver
Normal Appetite
Bowels and bladder are regular
No known allergies
Tobacco- chronic user- 1 pack khan over 3 -4 days since 24 years
Chronic alcoholic since 15 years of age.( 39 years)
Increased consumption since 30 years
Initially consumed 1-2 x a week with his cousins, 1 bottle.
at age 20, occupation changed to farmer, started drinking toddy , then arrack 180 ml per day,
4 times a week, whenever he felt pain.
After 2 years of drinking arrack- abstinent for 2 years.
Last 30 years- drinking whiskey 180 ml- strong urge- 180-360 ml/day
3-4 x 180 ml nights, 90 ml in morning if hands shake
continued til 20 years ago
10 years ago - jaundice, yellowing of sclera. Hospitalised and abstinent for 1 year
then again alcohol 2-3 x 180 ml almost daily increased if fearful
6 mo ago- jaundice, hospitalized with ascites , disoriented , recovered, hospitalised for 6 days and referred to higher centre and got well.
Swelling of the abdomen on and off for the last 5 months, abstinent for the last 5 months, since the last 2 weeks- 180-360 ml evening, 90 ml in the morning if hands shake.
Smokes 1 pack of KHAINI over 3-4 days.
FAMILY HISTORY:
NO SIGNIFICANT FAMILY HISTORY
PHYSICAL EXAMINATION:
GENERAL EXAMINATION:
NO PALLOR, CYANOSIS OR LYMPHADENOPATHY
ICTERUS, EDEMA, CLUBBING PRESENT
TEMPERATURE: 98 F
PR: 121 / MIN
RR: 22/ MIN
BP: 90/60
SYSTEMIC EXAMINATION:
ABDOMEN:
P/A: Distended, shifting dullness +,fluid thrill +, umbilical herniation +
DISTENDED
NON TENDER
UMBILICAL HERNIATION PRESENT
ORGANOMEGALY NOT APPRECIABLE
CVS: S1, S2 HEARD , NO MURMURS
RS: BAE +, No added sounds, CVS: S1, S2 heard, No murmurs.
CNS:DROWSY , AROUSABLE, SLURRED SPEECH
GCS- E 4 V5 M6
REFLEXES:
B/L REFEXES INTACT
INVESTIGATIONS:
CBP
RFT
LFT
USG ABDOMEN
CHILD PUGH SCORE;
10
MELD:
17
6 % 90 DAY MORTALITY
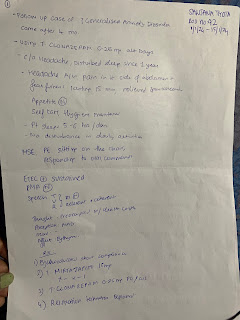
TREATMENT:

Comments
Post a Comment