1801006153- SHORT CASE
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
A 40 year old male, farmer by occupation came to the OPD with chief complaints of:
-loose stools since yesterday at 2 a.m.
-vomiting since today morning.
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic till yesterday evening when he suddenly developed loose stools yesterday night @ 2 a.m.
He has had 40 to 50 episodes of loose stools, large quantity, white coloured stools, foul smelling, non blood tinged.
The patient had 3 episodes of vomiting in the morning, with food particles as contents, non projectile, non bilious, non foul smelling relieved on their own.
For loose stools he went to a local RMP and received symptomatic treatment, he had similar episodes of vomiting and loose stools 10 years ago and got admitted for 1 week.
No history of food and water intake from outside.
No similar complaints in his family,neighbours.
No history of fever,cough or cold.
PAST HISTORY;
No history of DM,HTN,TB,EPILEPSY, CVA,CAD,THYROID DISORDERS
FAMILY HISTORY:
insignificant
PERSONAL HISTORY:
Diet-mixed
Appetite- decreased
Bowel and Bladder-Increased,increased burning micturition since today
Sleep-Disturbed
Addictions- none
GENERAL EXAMINATION:
Patient is conscious, coherent, cooperative.
Well oriented to time place & person.
Moderate build and moderately nourished
Pallor absent
No cyanosis, clubbing, icterus, lymphadenopathy
Vitals :
Bp -140/100 mmhg
PR -96 bpm ;
RR : 22cpm
Spo2 : 96 on RA
GRBS:128 mg/dl
ABDOMINAL EXAMINATION:
Inspection:
Abdominal distension is absent.
No scars, sinuses or engorged veins present,
Hernial orifices intact
Palpation:
No tenderness on Palpation
No organomegaly.
Percussion:
tympanic sounds in all 4 quadrants.
Auscultation:
Bowel sounds - PRESENT
CENTRAL NERVOUS SYSTEM
-No focal neurological deficits
-patient is conscious
-speech is normal
-no signs of meningeal irritation
-tone, power normal
-bulk is normal in both the upper and lower limbs.
CARDIOVASCULAR SYSTEM
S1 S2 heard
No murmurs.
RESPIRATORY SYSTEM:
Dyspnea-absent
No wheeze
Breath sounds - vesicular
No Adventitious sounds
INVESTIGATIONS:
HIV- NON REACTIVE
HBsAg RAPID Negative
Anti HCV Antibodies- NON REACTIVE
LFTs- NORMAL
HEMOGRAM- NORMAL, Hb- 13.6g/dl
LYMPHOCYTES: 11 %
SERUM ELECTROLYTES-
Urea- 24 mg/dl
CUE- Pale yellow, clear, acidic, 1.01 sp gravity, no sugars, bile salts, pigments or pus cells, RBCs or casts.
RBS- normal- 125mg/dl
USG:
2D-ECHO;
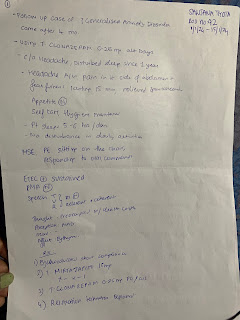
Treatment :
1.IV fluids : 2NS.1DNS.2RL@100 ml/hr
2. Inj.metrogyl 100 ml I.V TID
3.Inj.pan 40 mg I.V OD(BEFORE breakfast)
4.Inj.zofer 10 mg I V sos
5.Inj.Neomal 1 gm I.V sos
6.Tab.dolo 650 mg PO SOS
7.Tab.Red 100 mg Po/TID
8.Tab.sporlac-DS PO/TID
9.ORS in glass of water /SIPS WITH EACH EPISODES
10.Tab.OFLOX 300 mg PO/BD
11.BP.PR.RR.TEMP charting 4th hourly



Comments
Post a Comment