1801006153-LONG CASE
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
A 46 years old male came with complaints of abdominal swelling since 20 days, difficulty breathing since 20 days and swelling in both legs since 20 days.
Patient was apparently asymptomatic 6 years back when he had a thorn prick in the left foot, following which he developed a swelling of the left foot. He was diagnosed with necrotizing fasciitis and he underwent 4-5 episodes of dialysis.
Patient was apparently asymptomatic until 20 days ago when he noticed swelling of the both ankles and slight abdominal distension which was insidious in onset and gradually progressive, associated with shortness of breath which was relieved on medication and the patient was referred to KIMS for further evaluation.
No history of decreased urine output, chest pain, palpitations, PND, orthopnea.
Past History
History of 4-5 sessions of hemodialysis done in 2017 i/v/o necrotizing fasciitis.
Known case of Hyperthyroidism and Hypertension on irregular medication.
Family history:
No significant family history.
Personal history:
Appetite: Reduced
Bowel and bladder: Regular
Diet: Mixed
Sleep: Disturbed
General Examination:
Patient was conscious, coherent and cooperative.
Examined in a well lit room, well exposed and after taking informed consent.
Pedal edema: present since 20days of pitting type.
|
Pallor
|
Absent
|
|
Icterus
|
Absent
|
|
Cyanosis
|
Absent
|
|
Clubbing
|
Absent
|
|
Koilonychia
|
Absent
|
|
Lymphadenopathy
|
Absent
|
Bilateral pitting edema: grade 2
Vitals
|
Temp
|
A febrile
|
|
PR
|
84 bpm
|
|
BP
|
160/100 mm/hg
|
|
SpO2
|
98%
|
Systemic Examination:
CVS
On Inspection:
- Precordial area was symmetrical, no scars, sinuses seen.
-Chest wall movements were symmetrical.
-JVP-not elevated
-No parasternal heave
-No engorged veins
-Apical impulse not visible
Palpation:
-All inspectory findings confirmed.
-No local rise in temperature.
-No tenderness on Palpation.
-Apex beat felt at 0.5cm lateral to the mid clavicular line in 6th intercostal space.
Percussion:
-Heart borders percussed- Normal:
Auscultation:
-S1, S2 heard
-No murmurs heard.
Respiratory System:
On inspection:
-The skin over the chest is smooth, no engorged veins, no scars, sinuses.
-The trachea appears to be central in position.
Palpation:
-Symmetrical chest rise.
-Trachea central.
-No local rise in temperature, no tenderness.
Percussion:
-Resonant notes heard:
-Supraclavicular, infraclavicular, supramammary, inframammary,midaxillary, infraaxillary, suprascapular, infrascapular, interscapular.
Auscultation:
-BAE+
-No adventitious sounds heard.
-Normal vesicular breath sounds heard.
-Lungs clear.
GIT:
Inspection:
-Distended abdomen, longitudinally ovoid.
-Umbilicus central, inverted.
-No engorged veins, no scars, no sinuses, no visible pulsations.
-Hernial orifices intact.
Palpation:
-No local rise in temperature.
-Soft, non tender, no guarding, no rigidity .
-No organomegaly, hernial orifices normal.
Percussion:
-Dull notes on percussion over all 4 quadrants and in the flanks.
-Shifting dullness present.
-Fluid thrill present.
Auscultation:
-Normal Bowel sounds heard.
CNS:
-Higher mental functions normal.
-No focal neurological deficits.
-Sensory system: Normal
-Motor system:
-Tone, bulk, power: Normal.
-Reflexes 2+
Investigations :
Hemogram:
Test | Result | Units | Normal range |
Hemoglobin | 11.9 | gm/dl | 13.0-17.0 |
PCV | 36.3 | vol% | 40-50 |
RDW-CV | 16.9 | % | 11.6-14.0 |
RBC COUNT | 4.18 | millions/cumm | 4.5-5.5 |
RBC | Normocytic normochromic |
|
|
Serum chlorides- 106 mmol/L (98-109)
Serum creatinine - 3.7 mg/dl (0.9-1.3)
Test | Result | Normal Range |
Total bilirubin mg/dl | 0.87 | 0-1 |
Direct bilirubin mg/dl | 0.20 | 0.0-0.2 |
SGOT IU/L | 225 | 0-35 |
SGPT IU/L | 341 | 0-45 |
ALKALINE PHOSPHATASE | 242 | 0-25 |
TOTAL PROTEINS gm/dl | 5.1 | 0-45 |
ALBUMIN gm/dl | 3.2 | 53-128 |
A/G RATIO | 1.76 | 6.4-8.3 |
Electrolytes:
Blood urea- 110mg/dl (12-42)
Sodium- 139 mmol/l
ASCITIC FLUID ANALYSIS:
Ascitic fluid amylase- 39 IU/L (normal: 25-140)
LDH 218 IU/L (230-460 IU/L)
ECG changes suggestive of 4 chamber dilation:
peaked P waves in lead II suggestive of right atrial enlargement. (Not > 2.5 in this case)
evidence of left ventricular hypertrophy with large precordial voltages and an LV strain pattern in (I, II, V6)
Sokolov Lyon: < 35
Echo findings suggestive of 4 chamber dilatation:
All 4 chambers dilated, IVC dilated, moderate MR, moderate TR and PAH.
Report:Moderate to severe LV dysfunction, diastolic dysfunction.
Ascitic fluid tap was done.
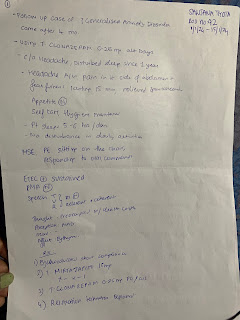
Treatment
On the day of admission
1.INJ LASIX 40MG PO/BD
2.T.SORBITRATE 5MG PO/OD
3.TAB NODOSIS 500MG PO/BD
4.TAB OROFER XT PO/BD
5.TAB SHELCAL PO/OD
6.TAB .ASPIRIN 75MG PO/OD
7.TAB.CLOPIDOGREL 75MGPO/OD
8.TAB ATORVAS 40MG PO/OD/HS
DAY 1
1.INJ LASIX 40MG PO/BD
2.T.SORBITRATE 5MG PO/OD
3.TAB NODOSIS 500MG PO/BD
4.TAB OROFER XT PO/BD
5.TAB SHELCAL PO/OD
6.TAB .ASPIRIN 75MG PO/OD
7.TAB.CLOPIDOGREL 75MGPO/OD
8.TAB ATORVAS 40MG PO/OD/HS
9.TAB MET XL 25MG PO/BD
DAY 2
1.INJ LASIX 40MG PO/BD
2.T.SORBITRATE 5MG PO/OD
3.TAB NODOSIS 500MG PO/BD
4.TAB OROFER XT PO/BD
5.TAB SHELCAL PO/OD
6.TAB .ASPIRIN 75MG PO/OD
7.TAB.CLOPIDOGREL 75MGPO/OD
8.TAB ATORVAS 40MG PO/OD/HS
9.TAB MET XL 25MG PO/BD
Provisional Diagnosis
-Heart Failure








Comments
Post a Comment