45 y/o Male with Acute on chronic Pancreatitis , chronic alcoholism
This is an online E- log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box.
CONSENT AND DEIDENTIFICATION : The patient and the attenders have been adequately informed about this documentation and privacy of the patient is being entirely conserved. No identifiers shall be revealed through out the piece of work whomsoever.
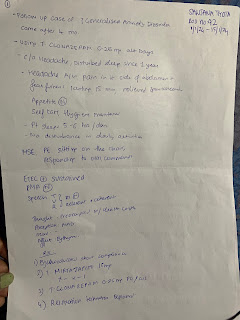
Pt came with c/o abdominal pain since 2 days
C/o vomiting since 2 days 6 episodes/day
HOPI
Patient was apparently asymptomatic 2 days back , then developed pain abdomen above the umbilicus, non-radiating , squeezing type, associated with nausea. Pt c/o vomiting, non-projectile,bilious,green color, liquid.
No h/o fever, diarrhoea
H/o melena since two days
No h/o blood in urine or urinary color change
No h/o blunt trauma to abdomen
History of past illness
K/c/o DM since 5-6 years
N/k/c/o htn, cad, cva, epilepsy,thyroid disorders
On medication: 12 u mixtard at night, metformin, sitagliptin 50 mg.
Personal History:
Occupation: lorry driver
Appetite - reduced due to alcoholism
Mixed diet
Bowels and Bladder regular
Alcoholic- since 20-25 years ago, drinks daily- 360-750 ml, sleep and appetite disturbances for 3-4 days of stopping alcohol.
Betel nut chewer- 1 packet for 2 days , same qty for 25 years
Family History:
No significant family history
Physical Examination:
General Examination:
Patient is c/c/c
No Pallor, icterus, cyanosis, koilonychia, Lymphadenopathy, edema
Temp: 98 F
Pulse rate: 84/ min
RR: 22 /min
BP: 110/70
SpO2: 98% at RA
GRBS: 254
Reflexes normal
Systemic Examination:
GIT:
Abdomen scaphoid in shape
No tenderness, no palpable mass, normal hernial orifices
No free fluid,
No organomegaly
CVS:
S1 S2 heard, no audible murmurs
CNS: No FND
Pt is c/c/c , speech is normal
CN intact, No motor or sensory deficits
GCS: E4 V5 M6
Investigations:
USG abdomen: Grade I fatty liver
Internal echoes noted in urinary bladder, likely cystitis, b/l raised echogenicity of the kidneys, correlate with rft, gall bladder sludge.
Investigations:
Diagnosis:
Acute on Chronic Pancreatitis
Treatment:
1. Inj. Tramadol in 100 ml NS stat
2.Inj. Ondansetron 8 mg stat
3.Inj. Thiamine 400 mg in 100 ml NS stat










Comments
Post a Comment